Preventing Bladder Cancer Recurrence with Chemo Wash
Before you get a TURBT, be sure to ask your surgeon if they are planning on doing a chemo wash.
If not, request them to do this.
Studies have clearly shown that a chemo wash after a TURBT helps prevent bladder cancer recurrence, or bladder cancer coming back again. I'll talk more about this further down in the article.
Article: What to Expect with a TURBT
After the bladder tumor is removed, more steps may be taken to try to ensure that the cancer has been completely destroyed. For instance, the tissue in the area where the tumor was may be burned while looking at it with the resectoscope. This is called fulguration. Cancer cells can also be destroyed using a high-energy laser through the resectoscope.
After a TURBT is performed, when you get a chemo wash, they will put a foley catheter inside your bladder. Then they will instill into your bladder a chemotherapy, most likely Gemcitabine or Mitomycin C, and have you hold it in your bladder for 1 hour. This is what is called a "chemo wash." It's washing out all of the loose cancer cells.
Article: Foley Cath, Straight Cath, Intravesicial Therapy - When to ask for a Catheter
When cancer is cut into, there are cells or "seeds" that come loose, which is called tumor seeding. You will void (pee) most of these out. But many doctors will do a one time chemotherapy instillation into the bladder right after the TURBT, so it will wipe out any potential cancer seeds. This is so hopefully there will not be another tumor growth, and that it won't spread to your lymph nodes.
Even if the TURBT removes the tumor completely, bladder cancer often comes back (recurs) in other parts of the bladder. This might be treated with another TURBT. But if the TURBT needs to be repeated many times, the bladder can become scarred and not be able to hold much urine. This can lead to side effects like frequent urination, or even incontinence (loss of control of urine).
A chemo wash after a TURBT has proven to decrease recurrence rates of bladder cancer.
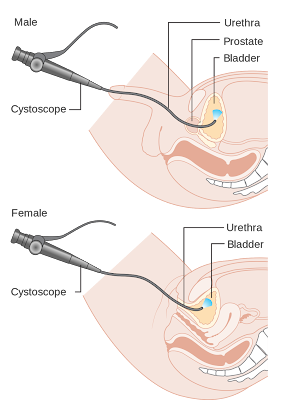
In patients with a long history of recurrent, non-invasive low-grade tumors (slow-growing tumors that keep coming back), the surgeon may just use fulguration to burn small tumors that are seen during cystoscopy (rather than removing them). This can often be done using local anesthesia (numbing medicine) in the doctor’s office. It's safe but can be mildly uncomfortable.
Sometimes, recurrence gets so frequent, and the cancer treatments so painful, people will choose to have their bladder removed.
Studies About Chemo Wash
After you get a TURBT surgery, it's a good idea to get a chemo wash of Gemcitabine or Mitomycin C. Having a chemo wash after a TURBT drops bladder cancer recurrence from 47% to 35%, shows one large clinical trial.
"Based on these results," Dr. Messing said in the article quoted below, "the addition of gemcitabine after surgery should be the new standard of care for patients with low-grade bladder cancer."
There are lots of other studies that show that using mitomycin C also decreased recurrence as well. However, there are concerns about the side effects of mitomycin C, as well as the availability and cost of the drug. Mitomycin C can be toxic if it leaks out of the bladder through a hole, and the drug can also cause severe rashes when it comes in contact with skin.
Gemcitabine, on the other hand, is a well-tolerated, readily available
drug that "comes at relatively little cost in terms of side effects or
expense," said Dr. Messing. The side effects were similar between the
two groups in the trial and were generally manageable, he added.
Article from National Cancer Institute (accessed 3/18/2022): New Treatment Approach Could Help Prevent Recurrences of Some Bladder Cancers
What to Expect with a Chemo Wash
When you wake up, your bladder will be more uncomfortable than a regular TURBT. It stings and your bladder hurts and spasms. The lining of your bladder has just been cut into and is raw. That chemo is irritating the hell out of your bladder. You just had a RIGID cystoscope go through your urethra, so your urethra is not happy about having a catheter in either.
It's held in there for an hour. For me, I was still pretty sedated, and so the pain was very controlled.
But you will still have an IV in, and you can ask for pain medication to help with this. The nurses gave me pain meds to help with the pain as I requested it.
They will take out the chemo after it's been sitting in your bladder for an hour. They will use what is called "chemo precautions" in which they will wear a gown, gloves, and splsh guard over their face. This is to prevent any chemo getting onto them.
Chemo can burn your skin.
So the first time you pee when you get home, you will still have chemotherapy in your bladder. It will be slightly more watered down, but it's still pretty potent.