For an intravenous pyelogram, you lie on your back on an exam table. The X-ray machine usually is either attached to or part of the table. An X-ray image intensifier — the part of the machine that obtains the images — is positioned over your abdomen. X-rays are taken before the contrast, and then the dye is injected and more images are taken at specifically timed intervals. Toward the end of the exam you may be asked to go to the bathroom and urinate. Then you return to the exam table, so that the health care team can get an X-ray of your empty bladder.
Pain Medications to Help With Bladder Cancer
🔶 Acetaminophen / Tylenol 1000mg every 8 hours: over the counter, and helps with pain, muscle aches, and fevers. Don't ever take more than 4 grams in 24 hours. This can be taken every 8 hours. This is also often in narcotics. Make sure you are adding up the TOTAL Tylenol usage for the day. Tylenol is processed in your liver, so can be taken at the same time as Ibuprofen.
🔶 Ibuprofen / Advil / Motrin 600 mg every 6-8 hours: over
the counter, and helps with pain, muscle aches, inflammation, and
fevers. This can be
taken every 6-8 hours. Ibuprofen is processed in the kidneys, thus it's
okay to take Tylenol at the same time (Tylenol is process in the
liver). Make sure you are drinking enough water to not stress your
kidneys. Ibuprofen can cause irritation and bleeding in your stomach.
This is classified as an NSAID (non-steroidal anti-inflammatory drug). DO NOT COMBINE WITH ASPIRIN!
🔶 Aspirin / Acetylsalicylic Acid / Bayer / 500mg every 6 hours : over
the counter, and helps with pain, muscle aches, inflammation, and fevers. Aspirin is processed in the kidneys, thus it's
okay to take Tylenol at the same time (Tylenol is process in the
liver). Make sure you are drinking enough water to not stress your
kidneys. Aspirin can cause irritation and bleeding in your stomach.
This is classified as an NSAID (non-steroidal anti-inflammatory drug). DO NOT COMBINE WITH IBUPROFEN!
🔶 Narcotics / Hydrocodone (Vicodin, Norco, Lortab) / Oxycodone (Percocet, Percodan):
These are all serious pain killers. You will get them after surgery if
you need them. I found that I needed on pill prescribed for BCG #12.
It's about a 4-6 hour window that the pain is just intolerable.
🔶 AZO / Pyridium / Phenazopyridine / Prodium / Pyridate / Baridium / Uricalm / Urodine / UTI Relief: a dye that works as a painkiller to sooth the lining of the urinary tract. It helps relieve pain, urgency, and frequency when urinating. It will turn your urine orange while it's in your system. This is totally normal. 😊 It does stain underwear permanently, so get some undies you can throw away. You can get this over the counter. If you want a pill with a higher dose (instead of taking many of the over the count types) you can have your doctor order it for you.
🔶 Anti-Anxiety :
There can develop some real anxiety around tests, procedures and
treatments. Lots of these things are painful, and so we develop anxiety
about them, often making the pain even worse. So take that anxiety
medication! Let someone else drive you to the appointment. 💗
Overactive Bladder or Bladder Spasm Medications
These are medications that help with bladder spasms or overactive bladder.
This can help after BCG therapy and after a TURBT. The ER or XL stands for
extended release. It makes it so you take the medication once a day, and
it release that medicine throughout the day.
🔶 Toterodine / Detrol
🔶 Oxybutynin (oxy-BYOO-ti-nin) / Oxybutynin ER / Ditropan XL
🔶 Trospium / Sanctura
🔶 Solifenacin / Vesicare
🔶 Darifenacin / Enablex
🔶 Fesoterodine / Toviaz
🔶 Mirabegron / Myrbetriq
Common Jargon, Types, Stages, and Grades of Bladder Cancer
🔶 Benign Tumor / Benign / Benign Cancer : a non-cancerous tumor. Benign tumors may grow large but do not spread into, or invade, nearby tissues or other parts of the body.
🔶 Cancer: A term for diseases in which abnormal cells divide without control. Cancer cells can invade nearby tissues and can spread through the bloodstream and lymphatic system to other parts of the body. You can only be certain a mass or tumor is cancer, by sending a sample of it to pathology.
🔶 Cancer Grade / Grade / Grade 1 = Low Grade / Grade 2 = Moderate Grade / Grade 3 = High Grade : there are three cancer grades. Grading is about how the cancer cells look under a microscope compared with normal cells. The more irregular the cells, the higher the grade. The higher the grade, the more aggressive the cancer is. The grade also tells how quickly the tumor is likely to grow and spread. The higher the grade usually the faster the tumor will grow and spread, and the more likely that the cancer will come back (recurrence) and progress (into a higher stage or metastasize forming other cancers in the body). Grading systems are different for each type of cancer.
🔶 Cancer Stage / Stage / Staging : The stage is determined by the cancer growth in the bladder wall and how far it has spread to nearby tissues and other organs, such as the lungs, the liver, or the bones. Staging is performing exams and tests to learn the extent of the cancer within the body, especially whether the disease has spread from the original site to other parts of the body.
🔶 Carcinogen: Any substance that causes cancer.
🔶 Carcinoma : Cancer that forms in the skin or lining of internal organs. In bladder cancer the lining of the bladder is called the urothelium.
🔶 Clean Margins: this means that when a tumor is taken out, at the outer edge of the tissue removed, there are no cancer cells found. If you have clean margins that will mean that that got it all!
🔶 Gene / DNA: Genes are the functional and physical unit of heredity passed from parent to offspring. Genes are pieces of DNA, and most genes contain the information for making a specific protein.
🔶 Malignant Tumor: a cancerous tumor. Malignant tumors can spread into, or invade, nearby tissues. They can also spread to other parts of the body through the blood and lymph systems. Also called neoplasm.
🔶 Metastasize / Mets / Metastasis / Metastases / Secondary Tumor / Primary Tumor: Metastasize means to spread form one part of the body to another. When cancer cells metastasize they form what is called a secondary tumor. The cells in the metastatic tumor are like those in the original (primary) tumor. Metastasis is the spread of cancer from one part of the body to another. The plural is metastases. Often with bladder cancer, if metastases occur, it will be in the liver, lungs, and bones.
🔶 Muscle-Invasive Bladder Cancer / Invasive Bladder Cancer / Infiltrating Cancer / Invasive Cancer: is when the cancer has grown into deeper layers of the bladder wall (muscle), and beyond, goring into surrounding and healthy tissues. These are more likely to spread to other organs and are harder to treat. This includes stage 2, 3, and 4, with being stage 4 extending past the bladder wall. These tumors have characteristically bad biological behavior and are capable of spreading to other parts of the body without much warning. Accordingly, physicians are constantly on the lookout for evidence of disease spread in patients with invasive bladder carcinomas (cancers in the endothelial lining of the bladder). Invasive cancers are less common than superficial ones, but they unfortunately spread to other parts of the body in about half of the patients who have this invasive disease.
🔶 Non-Invasive Bladder Cancer / Non-Muscle Invasive Bladder Cancer (NMIBC)/ Transitional Cell Carcinoma (TCC) / Urothelial (yer-o-THEE-ul) Carcinoma: I know, I know... that is whole lot of names! I wish they could simplify things. But when you see one of these named, it really means all of them. This is the cancer found in the tissue that lines the inner surface of the bladder called the urothelium.The bladder muscle is not involved, it has not grown into the muscle layer. That means it is stage 0 or stage 1. This is what about 90 percent of all bladder cancers are.
🔶 p53 Gene / p53 Tumor Suppressor Gene : This is a gene that can help prevent the development of tumors. Because p53 is essential for regulating DNA repair and cell division, it has been nicknamed the "guardian of the genome." In bladder cancer, alterations or this gene are common, occurring in about 50% of transitional cell carcinoma, also called non-invasive/ non-muscle invasive bladder cancer (NMIBC) or urothelial carcinoma. This is the most common form of bladder cancer (about 90%).
🔶 Pathology Report / Histology Report / Biopsy Report / Pathology / Pathologist / Histology / Histopathology / Patho / Histo:
pathology is the study of disease, and histology is the study of
microscopic structure of tissues. Histopathology is the study of
diseased cells and tissues using a microscope. It is the bridge between
science and
medicine. A pathologist is a board certified physician who studies body
fluids and tissues, identifying diseases by studying cells and tissues under a microscope. After
you get a biopsy (a sample of tissue or tumor) or a tumor
is resected (taken out), then that tissue or tumor is sent to
pathology. The pathologist will look at it under a microscope and tell
you if the growth is benign (non-cancerous) or malignant (cancerous). If
it is cancer the pathology report/histology report/biopsy report will
tell you the type of cancer, the
stage of the cancer, and the grade of the cancer. The pathology report
will also tell you that the surgeon had clean margins in the tissue
sample. You will often see people just use the word patho or histo when
describing these results. Example: "The patho showed NED" NED is no
evidence of disease by the way. 😊
🔶 Pre-Cancerous : A group of cells, tissue, mass, or tumor that may turn cancerous if left in place or untreated.
🔶 Primary Tumor: The original tumor or cancer in your bladder.
🔶 Prognosis: What your chance of recovery is.
🔶 Recurrent / Recurrence / Recur: To occur again. Recurrence is the return of cancer, at the same site as the original (primary) tumor in another location, after the tumor had disappeared. Recurrent UTI's mean you have a lot of urinary tract infections. More than what might be counted as "normal." Some studies have said that possible recurrent UTI's might be attributed to bladder cancer.
🔶 Refractory: In medicine, describes a disease or condition that does not respond to treatment.
🔶 Remission / Partial Remission / Complete Remission / NED / No Evidence of Disease:
remission is that signs and symptoms of your cancer are reduced or
gone. Remission can be partial or complete. In partial remission, some,
but not all signs and symptoms of cancer have disappeared. This could
mean the tumor is smaller. In complete remission, all signs and symptoms
of cancer have disappeared, although cancer still may be in the body.
NED stands for no evidence of disease. It means the patient is in complete remission.
🔶 Risk Factor: A habit, trait, condition, or genetic alteration that increases a person’s chance of developing a disease.
🔶 Secondary Tumor: A term used to describe cancer that has spread (metastasized) from the place where it first started to another part of the body. Secondary tumors are the same type of cancer as the original (primary) cancer.
🔶 Squamous Cell Carcinoma / Adenocarcinoma / Small Cell Carcinoma/ Sarcoma:
these are all very rare types of bladder cancers. Squamous cell
carcinomas originates from flat-shaped squamous cells found in the
tissue lining of the bladder. Adenocarcinomas originate from
mucus-secreting gland cells lining the bladder. Small cell carcinoma
occurs in less than 1% of all bladder cancers and is very aggressive and
doesn't respond well to treatment, often metastasizing or spreading to
other body parts. It come from nerve-like neuroendocrine cells in the
bladder. Sarcomas come from the bladder’s muscle cells.
🔶 Ta / Stage Ta / Ta0 / Superficial Bladder Cancer: This tells us how the tumor looks and that it is stage 0 (caught very early). It's a non-invasive (not in the muscle) papillary (it sticks out and looks like cauliflower or coral) carcinoma. This type of cancer has grown toward the hollow center of the bladder but has not grown into the connective tissue or muscle of the bladder wall. It is only in the urothelium layer (part that touches the urine) of the bladder. It has not spread to nearby lymph nodes or distant sites. This can easily be removed by a TURBT (a surgery where they go in through your urethra, and take out the tumor). The majority of bladder cancers are superficial, though these progress in only a minority of patients, they do usually recur.
🔶 Tis/ CIS/ Stage Tis / Tis / Carcinoma in Situ / Superficial Bladder Cancer: this tells us how the tumor looks and that it is stage 0 (caught very early). This tumor is flat. It's a non-invasive (not in the muscle) flat carcinoma. These cells are only in the urothelium layer (part that touches the urine) of the bladder. These types of tumors have a aggressive being higher grade, increasing the risk of recurrence (coming back) and progression (getting bigger and growing outside the bladder and spreading to other body parts). The majority of bladder cancers are superficial, though these progress in only a minority of patients, they do usually recur.
🔶 Tumor/ T / Mass / Neoplasm / Neoplasia : an abnormal mass of tissue that forms when cells grown and divide more than they should or do not die when they should. Tumors may be benign (not cancer) or malignant (cancer)
🔶 Upper Tract Urothelial Carcinoma / UTUC: While the majority of bladder cancers (approximately 90-95%) arise in the bladder, the urothelial cells that line the bladder are found in other locations in the urinary system. Sometimes these urothelial cancers can occur in the lining of the kidney or in the ureter that connects the kidney to the bladder. This is known as upper tract urothelial cancer (UTUC) correspond to a subset of urothelial cancers that arise in the urothelial cells in the lining of the kidney (called the renal pelvis) or the ureter (the long, thin tube that connects that kidney to the bladder).
Bladder Cancer Treatments, Surgeries, and Therapies
🔶 TUR / Transurethral Resection : Trans = by way of; urethral = urethra; This is usually done under general anesthesia (they put you to sleep for the surgery). A rigid cystoscope is used, along with resectoscope (see definitions below).
🔶
TURBT / Transurethral Resection of Bladder Tumor:
Trans = by way of; urethral = urethra; resection = to take out; bladder
tumor = a mass or tumor found in the bladder. It's a
surgery in which they remove a tumor in the bladder by going through the
urethra. This is usually done under general anesthesia (they put you to
sleep for the surgery). A rigid cystoscope is used, along with
resectoscope (see definitions below).
🔶 Resectoscope: A flexible instrument that can be inserted through the cystoscope sheath, or tube. The resectoscope has a wire loop that is used to remove the tumor. It also has a tool that uses an electric current to cut, remove, or destroy tissue and control bleeding. This is called fulguration.
🔶 Blue Light Cystoscopy:
It's a normal cystoscopy, but a special blue light on the end of the
cystoscope. This is a technology to detect and diagnose tumors in the
bladder. It
uses a
contrast solution that is absorbed by bladder cancer cells and makes
them turn
bright pink or red under a special blue light. This can be used during a
TURBT surgery, to find cancer cells that you human eye can't pick up
with just white light that is normally used with a cystoscopy. Some
doctors offices are also offering a blue light cystoscopy in their
offices. Many are not because of the increased expense for them. Many
insurance companies refuse to pay extra for a blue light cystoscopy.
🔶 Narrow Band Imagine Cystoscopy / NBI : A new technology that utilizes light of specific blue and green wavelengths. It's thought to improve the physician’s ability to detect small, non-muscle-invasive tumors that may not be seen with conventional cystoscopy. The technology takes advantage of the benefits of varying wavelengths of white light without the need for dyes or drugs. This can be done in the urologists office, or during a TURBT surgery.
🔶 Fulguration: Destroying tissue using
an electric current. This can be done during a cystoscopy, or during a
TURBT to destroy the bladder cancer.
🔶 Perforate / Perf / Perforation: Perforation
isa hole that develops thourgh the wall of a body organ like the
bladder. This can happen in surgery. If the bladder is perforated, then a
foley catheter is placed for several days, while the bladder whall
heals.
🔶 Resection / Excision: surgery to remove tissue or part or all of an organ
🔶 Incision: A cut made in the body during surgery.
🔶 BCG / Bacillus Calmette Guerin / Tice BCG: BCG is an active form of tuberculosis. Yes, you read that right. Tice BCG is a specific strain that is used in bladder cancer treatment. In the 1970's some scientists noticed that mice that had active tuberculosis, did not get cancer. Thus was born immunotherapy, a treatment that helps your immune system fight the cancer. BCG treatment is given to those with early-stage bladder cancer, stage 0 and stage 1. Those stages mean the cancer has not got into the muscle, and so it's called non-muscle invasive bladder cancer (NMIBC). BCG is instilled or inserted directly into the bladder, through a catheter (small flexible tube). BCG is the gold standard treatment used to treat early-stage bladder cancer. It is usually given once per week.
🔶 Immunotherapy / Cancer Immunotherapy / Biological Therapy / Biotherapy / Biological Response Therapy (BRM) : Treatment to stimulate or restore the ability of a person's immune system to
fight infection and disease. Also used to lessen side effects that may
be caused by some cancer treatments. There are many types of immunotherapy used with different treatments of bladder cancer. The most common type is BCG.
🔶 Catheter / Straight Cath / Self-Cath / Foley Catheter: a catheter is a narrow, flexible tube taht can be used to drain and collect urine from the bladder. It can also be used to infuse medication or fluid into the bladder. A regular catheter or straight catheter or the catheter used for self catheterization, is for a one time use only. A foley catheter has a balloon at the end of it. After the catheter is threaded into the urethra and then into the bladder, the ballon is inflated with saline. This catheter will stay in place for as long as needed. It does need to be periodically changed. The ballon stays inflated until the saline is taken out. The balloon keeps the catheter inside the bladder. A foley catheter might be used for many instances including after surgery if the bladder was perforated (a hole made in the wall), or if you can't urinate after BCG.
🔶 Maintenance BCG: The schedule of BCG includes an initial 6 weeks once per week, then 3 weeks (once per week) at 3 months, 6 months, 12 months, 18 months, 24 months, 30 months, and 36 months. All the doses of 3 weeks, are considered maintenance BCG doses.
🔶 Induction BCG: this the initial 6 weeks of BCG that are given after the TURBT. The BCG is given once per week.
🔶 Intravesical / Intravesical BCG / Intravesical Chemotherapy / Local Therapy: Local therapy is treatment that affects cells in the tumor and the area close to it. Intravesical therapy is a local therapy for bladder cacner. With intravesical therapy, the doctor puts a liquid drug right into your bladder rather than giving it by mouth or injecting it into your blood. The drug is put in through a soft catheter that's put into your bladder through your urethra. The drug stays in your bladder for up to 2 hours. This way, the drug can affect the cells lining the inside of your bladder without having major effects on other parts of your body. BCG, and chemotherapy are common medications used for intravesical therapy to treat bladder cancer.
🔶 Local Thearpy: Local therapy is treatment that affects cells in the tumor and the area close to it.
🔶 Systemic Thearpy: Treatment that uses substances that travel through the bloodstream, reaching and affecting cells all over the body.
🔶 Radiation / Radiotherapy / External Radiation / External-Beam Radiation: A cancer treatment that uses a machine to aim high-energy, high doeses of radiation rays at the cancer. Radiation therapy kills cancer cells, slows their growth by damaging their DNA, or will shrink cancer tumors.
🔶 Chemotherapy / Chemo: used to treat cancer as anti-cancer drugs. Often is cytotoxic (means that it damages or kills cells). Chemotherapy often is targeted for fast growing cells in your body. It can be given intravenously (IV, or in your vein), or intravesical (put directly into your bladder). That would include cancer, but unfortunately will also target your gut (thus the nausea and vomiting), as well as hair follicles, or the structures in the skin from which hair grows. Hair follicles are some of the fastest growing cells in the body.
🔶 Intravenous / IV :
a therapy in which medicaitons or fluids are given straight into your
vein. A device is put in your vein by inserting a needle into your skin,
and peircing the vein. The device will be taped and a dressing put over
it. This device is called an IV. How the medication is given is also
called IV or intravenous. For instance you will see written down Normal
Saline IV. That means that they normal saline will be given
intravenously.
🔶 Neoadjuvant / Neoadjuvant Therapy: Treatment given as a first step to shrink a tumor bofore the main treatment, which is usually surgery. Examples of neoadjuvant therapy include chemotherapy, radiation therapy, and hormone therapy. It is a type of induction (first or starting) therapy.
🔶 Adjuvant / Adjuvant Therapy: Additional cancer treatment given after the primary, or initial, treatment to lower the risk that the cancer will come back. Adjuvant therapy may include chemotherapy, radiation therapy, hormone therapy, targeted therapy, or biological/immunotherapy therapy.
Bladder Removal and Urinary Reconstruction Surgery Terms
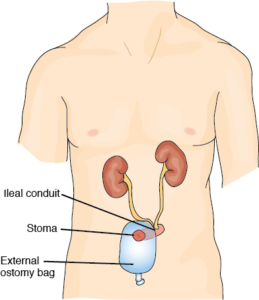
🔶 Cystectomy / Complete Radical Cystectomy (RC) / Complete RC / Partial RC / Segmental Cystectomy: Radical means total or complete. Cystis means bladder, and ectomy means removal. So a complete radical cystectomy is the total surgical removal of the bladder. When a radical cystectomy is performed, your surgeon needs to reconstruct the urinary tract in one of three ways so that your urine can be eliminated from your body: illeal conduit, continent cutaneous diversion/pouch, and neobladder. Partial cystectomy or segmental cystectomy (they are the same thing) is pretty uncommon, in which with the tumor, only a part of the bladder would be removed. If you want a more detailed and excellent description of this process and options available please visit this website from Bladder Cancer Advocacy Network (BCAN).
🔶 Urinary Diversion / Incontinent Urinary Diversion / Urinary Reconstruction / Continent Urinary Diversion: Urinary diversions are surgical
procedures that create new ways for urine to exit your body. These need
to be done because the bladder and other structures are removed. There are three surgeries
that do this. They are called illeal
conduit, continent cutaneous diversion/pouch, and neobladder.
🔶 Ileal Conduit (IC): This is the easiest and most common reconstruction. Your surgeon disconnects a short portion of your small intestine called the ileum. One side of the piece of ileum is attached to a skin opening on the right side of the abdomen and a small stoma, or mouth, is created. A conduit or a passageway between the kidneys and ureters and the urethra is made using the piece of the intestine - the ileum. The ureters (tubes that carry urine from the kidney to the bladder) are attached to one end of the ileum, while the other end of the ileum is attached to the stoma. The stoma is usually located close to the belly button on the right side. A plastic appliance called an ostomy bag, is placed over the stoma to collect urine. Because the nerves and the blood supply are preserved, the conduit is able to propel the urine into the appliance, or ostomy bag.
🔶 Ostomy / Ostomy Bag / Stoma / Urostomy / Ostomate: A
stoma is an opening or pathway that your surgeon makes, from the inside
of your body to the skin on the outside of your body. A urostomy is a
stoma made for your urinary system - so you can get urine out of your
body when your bladder has been surgically removed. Your urine will
drain into a bag, or ostomy bag, that you put around your stoma. You’ll
drain the bag as
needed. This is created and used in an Illeal Conduit surgery. There is
also a stoma with the continent cutaneous diversion surgery, but there
is no bag on the outside to hold the urine. There is a pouch made inside
the body that a catheter will access to get the urine out. Someone who
has a stoma is called an ostomate.
🔶 Wound Ostomy Continence Nurse / WOCN Nurse / WOC Nurse / Enterostomal Therapist: a registered nurse that is specially trained to take care of ostomies, and to teach their patients how to manage them is called a wound ostomy continence nurse or WOCN nurse or WOC nurse. They might also help the surgeon figure out the best location for your stoma. An enterostomal therapist is a health professional trained in the care of persons with urostomies and other stomas.
🔶 RC/IC ; Radical Cystectomy With Ileal Conduit: This is the most common urinary system reconstruction. This is the removal of the bladder, with an illeal conduit reconstruction of the urinary tract. You will often see people write RC/IC.
🔶 Continent Cutaneous Diversion / Continent Cutaneous Pouch (CCP) / Indiana Pouch Reservoir / Indiana Pouch: This is another method of reconstructing your urinary system, after bladder removal or radical cystectomy. Your surgeon reconstructs a continent reservoir or a urine "storage container," sphere or pouch, using part of your small and large intestine. The ureters are attached to one end of the reservoir, and the other end of the reservoir is connected to a small opening (stoma) in the skin of your abdomen. The reservoir stores urine and must be emptied periodically by inserting a small thin drainage tube (catheter) into the stoma, and then removing the catheter. No external bag is necessary.🔶 Urinary Pouch: A urinary pouch is created from a continent cutaneous pouch surgery. You’ll put a drainage catheter (thin, flexible tube) into the stoma several times a day to drain your urine.
🔶 Neobladder / Neobladder-to-Urethra Diversion: another method of reconstructing your urinary system, after bladder removal. Your surgeon uses a long piece of small intestine to create a continent reservoir to store urine. The surgeon reconstructs the tubular shape of the intestine an crates a sphere. The ureters are attached to one end of the reservoir, and the other end of the reservoir is connected to the urethra, the tube that carries urine out of your body, so you can pass urine in a similar way to what you did before surgery. You empty your reservoir periodically by relaxing your pelvic muscles and tensing your abdominal (belly) muscles.
🔶 Anterior Pelvic Exenteration / Anterior Exteneration: This is the standard operation to remove organs from your urinary and gynecologic (female) systems. This includes the removal of bladder, urethra, uterus, cervix, ovaries, and the anterior or front wall of the vagina. This operation has recently been modified so the urethra can be preserved. In addition, patients of childbearing age may wish to discuss with their surgeon techniques for preserving the uterus and cervix during a cystectomy (removal of the bladder). Because the bladder and urethra have been removed, this means you’ll need a new place for urine to leave your body. Your surgeon will connect your ureters to a new urinary collection system called a urinary diversion or urostomy.
















No comments:
Post a Comment