|
| TURBT of Female |
 |
| TURBT of Male |
What is a TURBT?
T - Trans, or by way of
U - Urethral, the surgery is done by going through your urethra, to reach the bladder
R - Resection, the medical term for surgically removing the tumor
B - Bladder, your organ that holds urine
T - Tumor, a growth
A TURBT is done to remove the tumor from the bladder, and also the doctor might biopsy some of the areas in your bladder. The surgeon attempts to remove all of the cancer cells from the bladder. It is often used to find out if someone has bladder cancer and, if so, whether the cancer has spread into (invaded) the muscle layer of the bladder wall.
TURBT is also the most common treatment for early-stage or superficial (non-muscle invasive, so stage 0 and stage 1) bladder cancers. Most patients (90%) have a superficial cancer when they're first diagnosed, so this is usually their first treatment.
Sometimes, a second, more extensive TURBT is done to better ensure that all the cancer has been removed. The goal is to take out the cancer cells and nearby tissues down to the muscle layer of the bladder wall.
They need to make sure they have clean margins. That means what they have cut out, they need to make sure the tissue is "clean" or free of cancer cells, where the tumor was growing. This is called having clean margins.
Biopsy
A biopsy can be done beforehand, or during or after the TURBT as well. This can be done after doing BCG, when you have red and angry patches in your bladder. Your urologist will want to rule out if the red patch is really a CIS cancer.
This literally just happened to me in Feb of 2022. I had a small Ta recurrence (low grade) and I had several red patches that the biopsies came back as chronic inflammation.
Most will just take the tumor out and then send it to pathology, where they will find out if it's cancer, the stage of the cancer, and the grade of the cancer.
Article: Pathology, Pathologists, Pathology Report and Bladder Cancer
That was the case with me for my first TURBT. We didn't know if the tumor we found in my bladder was cancerous or not, we just knew it needed to come out.
Surgery Process
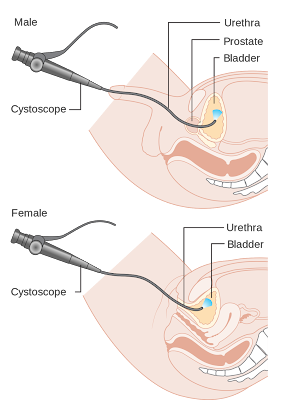
This surgery is done using an instrument put in through your urethra, so there's no cutting into the abdomen (belly). You'll get either
general anesthesia (drugs are used to make you sleep) or regional
anesthesia (the lower part of your body is numbed).
They use a thin, rigid cystoscope, called a resectoscope, in a TURBT. It's slightly wider than the flexible type that is found in the office of the urologist. It does not bend (thus the term "rigid"), and you are put under anesthesia to use this type. The scope has a wire loop at the end that's used to remove any abnormal tissues or tumors. It also has a camera, a light, and tube to suck out urine and blood and spray normal saline in as needed to enlarge the bladder, or wash away blood so they can see better.
After the tumor and tissue is removed, it is sent to the lab, or pathology, for testing.
Article: Difference Between Rigid and Flexible Cystoscopy
Preventing Bladder Cancer Recurrence with Chemo WashBefore you get a TURBT, be sure to ask your surgeon if they are planning on doing a chemo wash.
If not, request them to do this.
Studies have clearly shown that a chemo wash after a TURBT helps prevent bladder cancer recurrence, or bladder cancer coming back again. I'll talk more about this further down in the article.
Article: What to Expect with a TURBT
After the bladder tumor is removed, more steps may be taken to try to ensure that the cancer has been completely destroyed. For instance, the tissue in the area where the tumor was may be burned while looking at it with the resectoscope. This is called fulguration. Cancer cells can also be destroyed using a high-energy laser through the resectoscope.
After a TURBT is performed, when you get a chemo wash, they will put a foley catheter inside your bladder. Then they will instill into your bladder a chemotherapy, most likely Gemcitabine or Mitomycin C, and have you hold it in your bladder for 1 hour. This is what is called a "chemo wash." It's washing out all of the loose cancer cells.
Article: Foley Cath, Straight Cath, Intravesicial Therapy - When to ask for a Catheter
When cancer is cut into, there are cells or "seeds" that come loose, which is called tumor seeding. You will void (pee) most of these out. But many doctors will do a one time chemotherapy instillation into the bladder right after the TURBT, so it will wipe out any potential cancer seeds. This is so hopefully there will not be another tumor growth, and that it won't spread to your lymph nodes.
Even if the TURBT removes the tumor completely, bladder cancer often comes back (recurs) in other parts of the bladder. This might be treated with another TURBT. But if the TURBT needs to be repeated many times, the bladder can become scarred and not be able to hold much urine. This can lead to side effects like frequent urination, or even incontinence (loss of control of urine).
A chemo wash after a TURBT has proven to decrease recurrence rates of bladder cancer.
In patients with a long history of recurrent, non-invasive low-grade tumors (slow-growing tumors that keep coming back), the surgeon may just use fulguration to burn small tumors that are seen during cystoscopy (rather than removing them). This can often be done using local anesthesia (numbing medicine) in the doctor’s office. It's safe but can be mildly uncomfortable.
Sometimes, recurrence gets so frequent, and the cancer treatments so painful, people will choose to have their bladder removed.
Studies About Chemo Wash
After you get a TURBT surgery, it's a good idea to get a chemo wash of Gemcitabine or Mitomycin C. Having a chemo wash after a TURBT drops bladder cancer recurrence from 47% to 35%, shows one large clinical trial.
"Based on these results," Dr. Messing said in the article quoted below, "the addition of gemcitabine after surgery should be the new standard of care for patients with low-grade bladder cancer."
There are lots of other studies that show that using mitomycin C also decreased recurrence as well. However, there are concerns about the side effects of mitomycin C, as well as the availability and cost of the drug. Mitomycin C can be toxic if it leaks out of the bladder through a hole, and the drug can also cause severe rashes when it comes in contact with skin.
Gemcitabine, on the other hand, is a well-tolerated, readily available
drug that "comes at relatively little cost in terms of side effects or
expense," said Dr. Messing. The side effects were similar between the
two groups in the trial and were generally manageable, he added.
Article from National Cancer Institute (accessed 3/18/2022): New Treatment Approach Could Help Prevent Recurrences of Some Bladder Cancers
What to Expect with a Chemo Wash
When you wake up, your bladder will be more uncomfortable than a regular TURBT. It stings and your bladder hurts and spasms. The lining of your bladder has just been cut into and is raw. That chemo is irritating the hell out of your bladder. You just had a RIGID cystoscope go through your urethra, so your urethra is not happy about having a catheter in either.
It's held in there for an hour. For me, I was still pretty sedated, and so the pain was very controlled.
But you will still have an IV in, and you can ask for pain medication to help with this. The nurses gave me pain meds to help with the pain as I requested it.
They will take out the chemo after it's been sitting in your bladder for an hour. They will use what is called "chemo precautions" in which they will wear a gown, gloves, and splsh guard over their face. This is to prevent any chemo getting onto them.
Chemo can burn your skin.
Chemo Precautions for 6 Hours
About 6 hours after the chemo wash, you need to be aware there is still some chemo in your bladder. It will be slightly more watered down, but it's still pretty potent. It's a less concentrated dose, but it's still there.
So some simple things are recommended:
- Sit down on the toilet for urination, to decrease splashing
- After urination, rinse the head of your penis if you are a man (in the shower, or in the sink using a peri bottle - see below).
- If you are a woman, wash your labia, vagina area, and anus (anywhere the urine touched). You can do this with a peri bottle (see below) over the toilet.
- After urination, close the lid of the toilet before flushing.
- Flush the toilet twice.
- Drink plenty of fluids for 6-8 hours after treatment to flush the chemo out quickly.
Also, once you are home, don't use wipes! It will ADD to the dryness and irritation. There is alcohol in wipes. This will only cause further irritation.
Risks of a TURBT
The most common complications of a TURBT are bleeding, pain, urinary frequency/urgency, and spasms.
But there is also a possibility of urinary retention, infection, ureteral stricture, and perforation.
Other complications could be what can happen in any surgery - unexpected reaction to the anesthesia, developing a blood clot in your leg (deep vein thrombosis), or pulmonary embolism (where the blood clot travels to your lungs).
Side Effects of a TURBT
From what I have seen on bladder cancer forums, it varies widely how people react to TURBT's. I read from one patient that they were fine after just one day of recovery. Others have the full shabang and are not happy campers for 6-8 weeks.
I truly believe this has a lot to do with the size of the tumors, the temperament of your surgeon (I found out that a surgeon can be slower with insertion to help with urethral pain), your perception of pain, your age, your health, etc.
I have now had two different ones, from two different surgeons. I had pretty similar reactions. The second one was definitely easier than the first.
TURBT #1 I had a lot more pain. The tumor was much larger (3 cm). The pain lasted 7 weeks both my bladder and my urethra. The first two weeks were the worst.
TURBT #2 The tumor was a lot smaller (less than 1 cm). I had a lot less pain in my urethra but a lot more urgency, pain with urination, and urinary frequency. Before this TURBT I had 12 BCG treatments.
My surgeon specifically said he would be very careful with TURBT #2 and would slowly insert the rigid cystoscope, to help with the pain in my urethra. I was worried that these TURBTs were going to create permanent damage in my urethra.
I counted it up. In 16 months, my urethra was accessed with catheters and scopes 21 times!! You need to have a good working urethra if you are in the midst of cancer treatments.
The first two weeks were the worst. Pain lasted until week 4. I started BCG then so I can't tell you past that. Before I started the BCG my urine showed blood in it, which means I'm still bleeding from the TURBT 4 weeks after surgery. That makes sense, I was still having bladder pain and stinging and burning with urination (not like a UTI).
Bleeding, Pain, Urinary Frequency/Urgency, and Spasms
Bleeding, pain, and spasms after surgery is the most common side effect of a TURBT.
For me, with both the first and second TURBT, the bleeding was quite minimal, with of course the first couple days having the most blood in my urine. After about a week, I could no longer see blood in my urine.
After TURBT #2, at week 4 I was in the urologists office to start BCG. My urine showed some blood in there, because of the TURBT.
You will most likely experience pain during urination (stinging sensation), pain in your bladder, and pain in your urethra. I didn't know exactly where my urethra was (I'm a woman), like pinpoint the spot in my mind. After going through all of this... oh I know EXACTLY where it is!
The pain lasts 4-8 weeks depending on what was done and how extensive the tumor was, your perceptions of pain, and how quickly you heal.
For my first TURBT, urinary urgency and frequency were a serious problem the first couple of days. It feels like you have a UTI (urinary tract infection). It's not fun.
However, after my second TURBT, I had a lot more urgency and frequency for over a week. TURBT #2 was different for me because I had a chemo wash done the second time, and also I have been getting BCG treatments for the last 13 months. BCG is notoriously terrible to your bladder. I've had more urgency and frequency because of the BCG. It does seem more intense than my new "Post BCG" norm these days.
Article: BCG Information and Advice for Non-Invasive Bladder Cancer
Medications to help
There are so many medications that can help you with your urinary symptoms. Be sure to ask BEFORE the surgery for these meds.
Article: Bladder Cancer Medications for Symptom Management
Pyridium (over the counter called AZO) can be taken to help with these symptoms. My doctor gives me 200mg dose. It's a higher dose, and it sure helps!
Remember to take Tylenol and ibuprofen as well. This will help with the pain and also inflammation.
I've recently learned and experienced the pain relief of cannabis with these urinary symptoms after a TURBT and BCG. I can't believe how much it helps! You need more than just the CBD. You need the THC. Around 10mg (this depends on how often you use it, I don't use it hardly ever). It takes the pain away!
I've used narcotics to help with the pain after a TURBT, and cannabis does a better job.
Bladder spasms are also a normal part of all of this. Your bladder has been greatly messed with. When it's not happy sometimes it will spasm. Your bladder is a huge muscle. It has the capability to contract all at the same time. This is called a spasm.
Honesty, bladder spasms feel exactly like a really intense period or a really strong contraction during birth. They are not fun. They instantly bring tears and falling on the floor in pain.
Your doctor can give you medicine that can help with bladder spasms. I highly recommend taking this the first few days after your TURBT. My doctor prescribed me Oxybutynin (5mg ER, or extended release).
Urinary Retention
Some people get more blood than others, or for longer periods of time. If you have more blood, there are greater chances for large clots to form. Or sometimes, as your bladder is healing and sloughing off scabs, these scabs or blood clots and block your urethra. That makes it so you can't pee. Your bladder can't empty. This is called urinary retention.
I unfortunately had this after BCG #12.I didn't have the retention after a TURBT, but instead after BCG. It's the same in that you can't urinate, and it's an emergency. Click on the link below to learn more about this problem, and what it's like.
Article: I Can't Pee! BCG and Acute Urinary Retention
If you notice this happening, you need to immediately go to the ER. You will need to be catheterized, and possibly hospitalized depending on what is going on. There is a strong possibility, that if you are sent you, will be have a catheter still in place.
Some doctors recommend going home with an indwelling catheter. Some people don't get a choice to have a catheter or not. But this can help prevent urinary retention from happening. If you have a larger tumor, there will most likely be a lot more blood. I would recommend having a catheter in that case.
If there is a bladder perforation (the doctor accidentally makes a hole in the bladder wall), you will also have to have a catheter. It can be anywhere from 2-10 days depending on what your circumstances are.
Article: Foley Cath, Straight Cath, Intravesical Therapy - When to ask for a Catheter
Urinary Tract Infection
After a TURBT you can get a urinary tract infection (UTI), which is very common during this time that your bladder is healing and sloughing off scabs. It's hard because the "normal" side effects of a TURBT look exactly like a UTI.
If you have a fever, call your doctor. This most likely means you have an infection and need to be treated.
For me, by day 4-5, a strange things happens. My uncomfortable urinary symptoms got worse for about a week! So week two will feel really close to right after surgery. It's pretty miserable and intense! This happened with both TURBT's I had. I think this is because of the healing process.
With TRUBT #1, this was very concerning. Why would the symptoms be getting worse? I thought because of a UTI. I called my doctor and he ordered a higher dose of pyridium and also an antibiotic, assuming I had a UTI. He didn't even make me come in and pee in a cup. I guess that is how common a UTI is after having a TURBT.
The antibiotic didn't seem to help at all. I didn't have a UTI. The healing process was just doing its thing.This same thing happened with TURBT #2, but this time I just went along, knowing that was just what my body did.
No UTI's with TURBT #2 either.
If you had to have a formal bladder repair (enter through the abdomen instead of the urethra), then the entry wounds can also have a possible infection. So watch for redness, fevers, and smelly discharge or pus coming from the wounds.
Urethral Stricture
A urethral stricture is the narrowing of the urethra, or the tube you pee out of, going from your bladder to the outside of your body, causing an obstruction. The flow of urine is stopped up or slowed down significantly.
A stricture can be caused due to a transurethral surgery.
Symptoms of of urethral stricture include side or back pain (called flank pain), feeling of fullness (your bladder is full of urine!), abdominal pain, difficulty urinating or emptying your bladder, frequent urination, blood in the urine, cloudy urine, nausea, vomiting, fever, frequent UTI's, and pain gets worse with increased fluids or alcohol.
Many of these symptoms will be because of the TURBT. If you are continuing to have these kinds of symptoms 2 weeks after your TURBT, be sure to talk to your urologist.
If you are having difficulty emptying your bladder, or your bladder feels very full and you can't pee, you need to go to the ER immediately. This is an emergency!
Personally, I was not told that this was a possible side effect. My urethra hurt for 7 weeks after the TURBT #1. I was really shocked by this!
Thankfully, I do not have ureteral strictures. My urethra did heal, without having problems. In the last 16 months, my urethra has been accessed with scopes and catheters 21 times!
With TURBT #2, I had a new urologist. This time a urologist oncologist. His demeanor was so different from my first urologist. I had to change doctors due to insurance issues. I'm so glad I did! My second Urologist is better than the first in EVERY way!
This included my second surgery. Feb 2022, we found some new tumors, and had TURBT #2. I had a conversation with my new urologist, Dr. Liam McLeod. I told him about my experience with my urethra from the last surgery, and I was worried that with more surgeries going through my urethra, I could really damage it. He told me that when accessing my urethra, he would be extra careful. He would go slower, use more lubrication and numbing gel, and be more gentle.
Well it worked! My urethra is doing so much better than with TURBT #1. I still have pain, but it's a lot less.
 |
| Left Bladder Dome Perforation (hole) |
Bladder Perforation
A possible risk with a TURBT is bladder perforation, or otherwise putting a hole in your bladder wall. They are going in to take out a tumor. If they cut too deep, it could go through the bladder wall.
If your bladder is perforated, you will wake up after surgery with a foley catheter in. You will need to keep the catheter in continuously for 4-10 days during the time that your bladder wall is healing and sealing itself off.
Your doctor really doesn't want this to happen, and of course we don't either! If what they are cutting out is cancer, and the bladder is perforated, then cancer
cells could leak out of the bladder in the urine, and seed into the
walls of your pelvic cavity (called the peritoneal or intraperitoneal cavity). To prevent this seeding, the catheter keeps the bladder almost continuously empty of urine, decreasing the chances of tumor seeding by urine leaking outside the bladder.
If the perforation is large enough further steps would need to be taken. During the surgery, you might have to get a cystogram (x-ray of the bladder, possibly using fluroscopy to find out how extensive the hole in the bladder wall is. It would make your urine look like it's glowing when you take an x-ray). The cystogram would help make sure the repair is thorough.
Additionally, if the perforation is really large and it extents into the peritoneal cavity, then a formal bladder repair may need to be done by either an open surgery (slicing a hole in your abdomen to get to the bladder) or laparoscopic (they make 2-5 tiny holes to get in there and do the surgery).
If they had to do a formal bladder repair, then you might have a drain that comes out of your abdomen (intra-abdominal drain), in addition to the foley catheter that comes out of your bladder.
Both the second and first TURBT this didn't happen to me.
Bladder Healing
Your bladder is really quite remarkable at healing. My husband is an Emergency physician. He once had a person's bladder explode in a car accident - it perforated or popped, because of the pressure of the urine in his bladder during the car accident! What was interesting, is they didn't have to sew it back together. They just put a catheter in for a week while it was healing.
Your bladder is awesome! I had no idea it has such healing capabilities!
WaitingWe have to wait for the urologist to get us in for a cystogram. We
have to wait for a surgery date. We have to wait for results. We have to
wait for the insurance company. We have to wait for the BCG. And on and
on!
Wait, wait, wait, wait!
When you think you have
cancer or know you have cancer, and you have to wait... oh it is one of
the worst things I have ever gone though. Life and death are in the
details.
The weeks prior to surgery were probably some of the
most difficult days of my life. I found out on October 27th that I had a
tumor growing inside of me. The next opening for surgery was Nov 23 -
what an agonizing 27 days!!!
The stages of grief were in full swing! I didn't stay in any of the stages for very long, it was quite the roller coaster ride - anger, denial, depression, shock, testing, bargaining, and even the start of acceptance.
We didn't know for sure this wasn't cancer, but the
fact that my urologist with over 30 years experience said I have the
classic look of bladder cancer, was pretty convincing.
I
would have days in which in my mind, I would pretend I was dead. My
husband later told me that he was doing the same thing. He was going
through the same stages that I was going through.
What would life look like with me not here?
Is this really happening to me? Did they really find a tumor or was that something else? What would my husband do as a widower of three young children? Would he move to be closer to family to get more support? Is everything in my life insurance up to date? Oh goodness, maybe I should have had a bigger life insurance policy!?!
Am I going to have to do
chemo? Am I going to have to pee into a bag the rest of my life? Am I going to lose my hair? I'm
already dealing with suicidal depression, how can I find the strength to
do this? I'm so angry this is happening to me and my family! Why cancer
when I have no risk factors!?! I'm 41 years old! I'm a woman! I don't
smoke! I have no history of cancer in my family!
Maybe I
really don't need to do any of this. Maybe my urologist doesn't know
what he's doing and he is just wrong. Maybe I should just let the cancer
take me? I really don't want to go through treatments. This sucks! All
of this really, really, sucks! All options are not the options that I
want! I have no control or choice over this! I don't want to get out of
bed! I don't
want to do anything! What's the use?
My moods and thoughts would vacillate dramatically and violently, sometimes within days and sometimes within minutes. I was crying one minute, screaming another, praying another, laughing another (not this one so often) , completely numb another, in complete denial another, so full of joy that I'm alive another, and so on.
It felt like I was not in control in any way! I was at the mercy of my doctor, and most of all God. What plans did God have for me? Where was God in all of this?
The
moments I was
able to come to a glimmer of acceptance was when I processed this idea.
We didn't know what this was, it didn't help to stress about it now or
to go to worst case scenario. Truly, I have no control over any of this.
God has got this. He is in EVERY detail of our lives.
I
had no control. This was not up to me. I would follow the protocols
that my doctor put in front of me, do my treatments, do the surgery -
the rest was up to God.
I would literally imagine in my
mind, putting the cancer into a ball of light, and then handing it over
to God. This would really give me peace. It helped me process, keep me
calm, and keep perspective.
I couldn't believe that it took 4 weeks to get me into surgery. How much more did that tumor grow in that time (come to find out not much)? COVID-19 was in full-swing again. Everything was completely shut down again.
Everything moves so slowly! My urologist is well-known and knows what he's doing. He's so busy because he has so many patients seeking after his expertise. I was willing to wait to get this done right.
For the rest of the article about Waiting and Staying Present with Bladder Cancer click on the link.
 |
| Gwen on Day of Surgery |
November 23, 2020 - surgery day. It was the Monday before Thanksgiving. I couldn't think of better timing for this surgery. Thanksgiving has always been one of my favorite holidays. Focusing on all the blessings in your life, and how good God has been to you and your family - I needed it more than ever!
Several days before the surgery, you might need to have a COVID test. I did with the first one. The second one I didn't because I had COVID 4 weeks before.
As with any surgery, they have you stop drinking and eating at midnight the night before.
One hospital had me take a shower the night before, and put clean sheets on my bed.
The second hospital had me take a shower the night before and then use some chlorhexidine wipes to clean myself with. They still had me get into clean clothes and change my sheets.
The morning of, I think I was in a bit of denial. I was very numb. I knew what needed to be done, and so I did it.
Shower with special cleanser, check. Braid my hair so it wasn't in my way or the nurses and doctors - check. Double check that I had everything I needed to go to the hospital - check. Say a prayer of protection and gratitude - check.
Cancer truly gives anyone perspective. It really does make each day a blessing that you are alive.
TURBT #2 was not as traumatic for me. I had been here and done that. I was still going through another greiving process (who wants to have a recurrance!?!?!), but I had learned better to stay present and roll with the punches. I had learned how to give myself plenty of space to feel what I needed to feel.
When you get to the hospital they make you pee in a cup. They had me use another set of chlorhexidine wipes to clean my whole body with, and get into a hospital gown. They started an IV. My awesome hubby put my hair into a braid.
Then... you wait! I waited for about 45 minutes. Luckily because this one wasn't during 2020 crazy COVID panic time, my husband was allowed to wait with me. It was really nice to have his love and support.
Telling Others About Your Tumor or Cancer
I was hesitant at first to tell many people about the tumor. We didn't have much information about it at this time, and I wasn't sure how I felt about telling people.
I always heard that people will start treating you weird if you tell them you have cancer or a tumor. I was still in the processing stage, and just didn't know what I wanted to do. Once word is out, you can't take it back. I wanted to do this carefully and deliberately, if I chose to tell others.
I had not told my children yet, because I needed more information first. I needed more time to process it, so I wasn't so scared. I wanted to be able to be confident in front of my children because I know that they will take cues from me.
So I told my husband, my mother, my siblings, and my closest friends. I was grateful that I did. I needed that love and support. I was also grateful that I waited to tell my children. Knowledge is everything. I knew they were going to have so many questions, and I wanted to know what this was, what my chances were of surviving this were before I talked with them.
The morning of my TURBT surgery I texted about what was going on to my small group of friends and family, and I had a bunch of texts come back with well-wishes, and lots and lots of prayers! None of us could do much but pray.
I felt loved and supported, and that meant everything! I can't even begin to tell you the peace that came upon me. It was powerful and profound. I know it was because of the prayers that were fervently being said by me, my family, and my friends.
God it good.
God is there for you in your trials, your terrifying moments of life, your pain and suffering. You just have to ask!
Surgery
I checked in as instructed, and they took me back to my room. Took vitals, peed in a cup, took labs, started an IV, changed into the hospital gown, and waited.
The doctor swung by to say hi and to see if I had any questions. I signed all sorts of paperwork. The anesthesiologist came by to ask about previous times I had been under general anesthesia.
Then it was time! They were ready to take me back.
The OR (operating room) was cold, and I scooted onto an incredibly hard table, that had this HUGE machine right over the bed. They told me it was an ex-ray machine in case they needed to x-ray during the surgery.
They asked me to start counting, I don't think I got past three or four. They were giving me medicine to go to sleep.
Next thing I know I'm in the PACU (Post Anesthesia Care Unit), well I didn't know that for sure. That was my second question, after the most important one!
"Do I have a catheter in?"
The nurse smiled at me.
"Nope. No catheter."
"Is this PACU?"
"Are you a nurse?"
"I was forever ago."
"Yes, this is PACU. You are waking up very well. The surgery went well. You will be out of here real soon."
In PACU they asked if I needed a pain medication. I told them no. I don't like how narcotics make me feel. I wanted to see how bad the pain was going to be, and see if I could do this without pain meds. The cystoscope in the urologists office (the flexible kind) was really not that bad. I was hoping that was the case here.
It wasn't!
I was soon taken to a recovery unit. I asked if I could stand. I was super antsy, and I just wanted to get out of there!
I started drinking water like mad. I was super thirsty. It felt like I urgently needed to pee. They told me that was just the pain from the surgery.
I waited for about 10 minutes, feeling like soon I was going to wet myself if I didn't try and pee.
So I tried. Can you say OUCH!?!?!
It felt like the worst UTI (urinary tract infection) ever! Just a tiny amount of pee and blood came out.
I've had a ton of UTI's in my life, and the pain always gets better with drinking more water. So that was my go-to idea. So I started drinking as much water as I could without barfing.
I had to pee in another 10 minutes. Again it felt like I was going to wet myself if I didn't go. Again so much pain.
That is when I decided it was time for narcotics! I don't need this pain! Drinking water actually felt like it might be making things worse! Everything was so irritated and it just needed rest, not crazy amounts of urine going through it.
So I stopped the excessive drinking of water. Normal amount of water is good - just not too much!
If I ever have to have another TURBT, I will ask for narcotics right off after surgery.
Then came the waiting for the drugs to start working. I don't know about you, but that terrible UTI pain is the worst. It's all you can think about. I need to pee, I need to pee, I need to pee. So I start rocking back and forth, walking back and forth in my room. One minute at a time. I can get through this!
Within 20 minutes the narcotics are starting to work - thank goodness!! What a blessing pain medications are.
The urgency and frequency feeling start to subside. It still burns when I pee, but not as bad.
My husband shows up, and we check out. We fill my prescriptions for a narcotic (I think there were only 3-6 pills given?), an antibiotic (to help prevent a UTI), and pyridium (it helps with the pain and urgency with urination).
We go home.
Recovery
As with all surgery, it's going to wipe you out, for much longer than you anticipate.
For me, the first week and a half to two weeks, I didn't have the capacity to be able to take care of others. I just rested (besides the constant peeing), and focused on getting better. Your energy will be much lower.
Keep yourself well hydrated, but don't crazy overdue the water. It's not like with a UTI. When I have a UTI the more water I drink the less pain I feel. That is not the case with this. However, good hydration will help with healing.
Eat lots of fruits and veggies and protein to help support your body in healing. Cut out the sugar and processed foods. That junk is just feeding cancer!
The pain with urination, urgency, frequency, was BAD for the first two weeks! In fact, after the first week, the pain seemed to worsen for a week or so. I thought it was a UTI. I called the doctor, and he said that this is a very common thing to happen as you are healing from a TURBT.
During this recovery time, I wear a menstrual pad. The Pyridium turns your urine orange, and stains everything. A pad can help protect your underwear.
The pain, urgency, and frequency can also cause dribbles of pee. The menstrual pad catches that and it's helpful. Overnight, I have not had any issues of incontinence.
I don't know if that would be different for men, or for older adults.
Your bladder will slough off scabs as it's healing. This can let bacteria grow, and cause a UTI. Your urine will be bloody for several days (I'm writing this 7 months later, I don't remember how long, but I know it was a least several days).
I took the antibiotics prescribed for the UTI, and it didn't help anything. I realized it wasn't a UTI - this is just how a post TURBT feels! OUCH!!
So if you have ever had a UTI, you will know what to expect.
After 2 weeks, it only feels like a UTI when you pee. You don't have the urgency or frequency like a UTI. You won't be constantly feeling like you have to pee. But every time you pee, expect pain.
I still had the pain - burning and stinging for 7 and a half weeks after surgery.
What was really surprising for me was that my urethra was still hurting after 7 weeks! It took just as long as my bladder to heal.
I'm not sure if that is just me or not. But it was terrible! My urethra was obviously damaged during the TURBT. Before this surgery, I didn't really know where my urethra was. I knew anatomically where it should be, but I couldn't feel it.
Between the TURBT and BCG - my goodness, I know where it is! I am fully aware of my urethra. It has served me so well and it has been through so much.
My doctor wanted a full 8 weeks of healing before starting BCG therapy. My bladder and urethra felt fantastic by week 8! Just in time to start BCG! LOL!